Supporting HIV Research From Cell to Society
Michael Stirratt, Jeymohan Joseph, Christopher Gordon, and Dianne Rausch on behalf of the NIMH Division of AIDS Research
• 75th Anniversary
For 75 years, NIMH has transformed the understanding and treatment of mental illnesses through basic and clinical research—bringing hope to millions of people. This Director’s Message, guest written by NIMH’s Division of AIDS Research, is part of an anniversary series celebrating this momentous milestone.
NIMH is currently celebrating its 75th Anniversary. Did you know that NIMH’s 75 years of mental health research includes over 40 years of HIV research? NIMH first received funds for the specific purpose of studying HIV and AIDS in 1983 and was one of the earliest NIH institutes to respond to the AIDS crisis, due to the many important connections between mental health, behavior, and HIV.
Over these 40 years, NIMH's contributions to HIV research have been numerous and meaningful. Leading these efforts is NIMH’s Division of AIDS Research (DAR). The work funded by DAR has touched every aspect of HIV, from understanding the virus at the cellular level to helping individuals manage their medications effectively to supporting community health practices and reducing societal stigma.
Working toward an HIV cure at the cellular level
Although we don’t yet have a cure for HIV, finding one is a priority for NIMH. We are working toward this goal by funding research that increases our understanding of HIV—and our ability to combat it—at the cellular level.
The human body is made up of trillions of cells, and HIV interacts with them in different ways. To cure HIV, we must first understand how the virus enters, impacts, and spreads across different cell types.
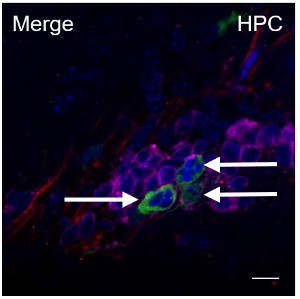
One example of this research is an NIMH-funded study that showed that HIV can enter brain cells, replicate there, and then spread to cells in other parts of the body. The finding that brain cells can spread HIV to the body underscores the importance of the brain in efforts to eradicate HIV. However, developing medications that target the brain presents a challenge because the blood-brain barrier—a protective layer of tissue surrounding the brain—prevents many HIV medications from reaching it.
Eliminating HIV from the brain is difficult, but a proof-of-concept study funded by NIMH showed that it is possible. Researchers were able to eliminate HIV from the brains of mice using novel gene-editing techniques in combination with long-acting forms of HIV treatment—an important first step toward developing treatments that can be used in humans.
Researchers are even using exosomes, tiny nanoparticles capable of being taken up by cells, to try to eliminate HIV from the body. In an NIMH-funded study , researchers used exosomes to deliver a novel protein into the cells of mice with HIV. The protein attached to HIV’s genetic material and prevented it from replicating, resulting in reduced levels of HIV in the bone marrow, spleen, and brain. The findings demonstrate another promising technique that could one day be used to eliminate HIV (and possibly other diseases) from the human body.
Reflecting NIMH’s ongoing commitment to advancing the development of HIV treatment and cures, our institute co-sponsors the Martin Delaney Collaboratories for HIV Cure Research . This flagship NIH program brings together 10 scientific collectives to accelerate research on cellular mechanisms and strategies for curing HIV.
NIMH-funded research has expanded our knowledge of how HIV interacts with our body at the cellular level, opening the door for the development of new treatments for HIV and bringing hope that one day, we may have a feasible cure for this virus.
Helping people use and benefit from lifesaving HIV medications
Although there is currently no cure for HIV, we are fortunate that there are safe and effective medications for HIV treatment and prevention. Research has shown that people with HIV who start treatment and stay engaged in care have a life expectancy close to that of people without HIV. However, this requires people to consistently take HIV medications for a lifetime, which is challenging for many. With NIMH support, researchers are developing programs to help people with HIV stick to their treatment plans, leading to better health over the long term.
One recent example is a study funded by NIMH in which researchers developed a brief counseling program that nurses could deliver to HIV patients in South Africa who were experiencing depression and uncontrolled HIV. The program, which included techniques from cognitive behavior therapy, helped reduce participants’ depressive symptoms, increase medication adherence, and improve HIV viral control. Further studies showed the program was cost-effective and likely to improve life expectancy.
There are also safe and effective drug regimens to prevent people from acquiring HIV, called HIV pre-exposure prophylaxis, or PrEP . NIMH-funded research generated some of the first behavioral interventions that can increase and sustain PrEP use. These include a program that provides interactive text message support for PrEP use (“PrEPmate”). When tested with young sexual minority men in Chicago (most of whom were Black or Latino), PrEPmate more than doubled the odds of PrEP adherence and retention.
The U.S. Food and Drug Administration has approved new long-acting forms of HIV treatment and PrEP. These treatments are administered through intramuscular injections on a monthly or bimonthly basis, providing an alternative to daily pill regimens. NIMH continues to encourage the use of multilevel research that helps improve the delivery and use of new long-acting HIV regimens, helping people live longer, healthier lives.
Advancing community- and society-level approaches to HIV
HIV not only affects individuals but also entire communities. Community-level influences, such as stigma, can affect the use of HIV testing, prevention, and care. NIMH is committed to supporting research to develop HIV health promotion strategies that are delivered at a larger societal level.
NIMH Project Accept is a key example. Conducted in 48 communities in Africa and Thailand, Project Accept is the largest and most ambitious community-level HIV study supported by NIMH to date. The study capitalized on the global reach of the HIV Prevention Trials Network (HPTN) to test whether mobilizing communities could improve the uptake of HIV testing and reduce HIV transmission.
The study showed that a community mobilization strategy, which involved engaging residents in festive public events with messaging about uniting to address HIV and offering free HIV testing, dramatically improved the uptake of HIV testing and found more people in the community with HIV. The mobilized communities also showed modest reductions in new cases of HIV.

NIMH Project Accept helped change the conversation by highlighting the importance and value of communities in addressing HIV. It heralded a broader and ongoing effort to decentralize and destigmatize the delivery of HIV testing, prevention, and care by moving these services out of hospital clinics and into local neighborhoods and community locations.
Conducting large-scale research like NIMH Project Accept requires collaboration with many groups. DAR routinely partners with other NIH Institutes, Centers, and Offices, including the NIH Office of AIDS Research and the National Institute of Allergy and Infectious Diseases Division of AIDS . NIMH also collaborates with other federal agencies to advance research projects and initiatives related to HIV, such as the Centers for Disease Control and Prevention Division of HIV Prevention and the Health Resources and Services Administration HIV/AIDS Bureau . These partnerships help increase the reach, scope, and real-world impact of NIMH-funded HIV research.
Remembering lives lost and committing to a future free of HIV
World AIDS Day is December 1, 2023, and its theme is “remember and commit.” At NIMH, we honor the lives of the more than 40 million people lost to HIV/AIDS worldwide and commit to advancing research from cell to society to help end this pandemic and relieve the burden of HIV. We invite you to join us—whether you are interested in NIMH-sponsored HIV research opportunities or learning more about DAR's work on HIV and AIDS. Working in partnership, we can turn the tide on HIV together.
From cells to society, NIMH has been at the forefront of supporting HIV research and improving the lives of those living with this virus. Today, we are proud to highlight a few of the many vital contributions that NIMH has made to HIV research.
Learn More
- HIV and AIDS and Mental Health: Learn basic information about HIV and mental health on this NIMH health information page.
- HIV Basics : Learn about HIV and HIV testing, prevention, and more on this page from the Centers for Disease Control and Prevention.
- Global HIV & AIDS Statistics — Fact Sheet : See statistics about global HIV and AIDS on this page, created by the Joint United Nations Programme on HIV/AIDS.
- More detailed scientific information about HIV can be found in this Nature Reviews journal article .
- Please feel free to subscribe to the NIMH Division of AIDS Research monthly newsletter by sending an email to darcommunications@nih.gov.